In this issue:
Welcome to the first issue of STIEF News for 2022 and International HPV Awareness Day!
- International HPV Awareness Day
- National hero wins Scientific Freedom and Responsibility Award
- Herpes and me, six months on – a consumer perspective
- Herpes Helpline Q&A – herpes and pregnancy
- Aotearoa NZ STI Guidelines for Primary Care
- Conversations with young patients about sex – Goodfellow podcast with Dr Cathy Stephenson
- STI media mentions:
International HPV Awareness Day
STIEF has partnered with the International Papillomavirus Society to promote this day as part of our shared commitment to raise the profile of HPV (human papillomavirus) as a cancer causing virus and provide the information and knowledge that people need to take action to reduce HPV-related disease.
This year the campaign is focused on delivering a world with one less worry - #onelessworry.
How can I protect myself against HPV-related disease?
- Vaccination: If you are under 27 and haven't been vaccinated - do it! Vaccination prior to sexual contact is the most effective way to protect against HPV and HPV cancers. Research shows that vaccination prevents almost 90% of cervical cancer cases.
- Cervical cancer screening: While most HPV-related cancers cannot be screened for, the cervical screening programme detects cell changes on the cervix. For all people with a cervix, inclusive of those who identify as men (transmen), regular cervical screening will ensure early detection and treatment of HPV-related abnormal cells and prevention of most cervical cancer.
- Condom use: Condoms, used correctly from start to finish, offer some protection against HPV – the more you use them the more protected you are. But as condoms don’t cover the whole genital area, you can still become infected.
Together we have the opportunity to help eliminate HPV-related cancers for future generations!
Go to our International HPV Awareness Day web page >
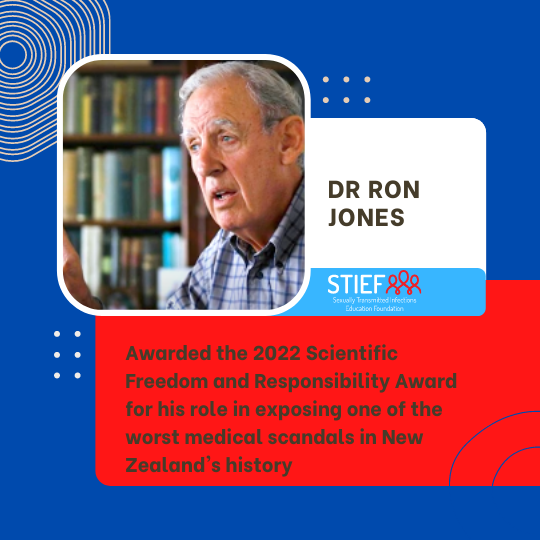
National hero wins Scientific Freedom and Responsibility Award
We are extremely proud of one of our founding board members, Dr Ron Jones, for being awarded the 2022 Scientific Freedom and Responsibility Award from the American Association for the Advancement of Science (AAAS). This is in acknowledgement of his role in exposing the National Women’s Hospital ‘Unfortunate Experiment’ involving women with cervical carcinoma in situ (CIS).
Herpes and me, six months on - a consumer perspective
In a follow-up from her candid story about her herpes battle, Sarah is back with what’s happened since – and to say she’s been blown away is an understatement.
Herpes Helpline Q & A
The Herpes Helpline regularly receives enquiries from people struggling with the shock, shame and confusion resulting from a new genital herpes diagnosis. This is an opportunity for the Helpline nurse counsellors to educate people that herpes simplex (either facial or genital) is, in most situations, a medically insignificant infection. It is simply a skin condition (more commonly known as cold sores) that many of us have and if it is problematic there is effective treatment available. In the vast majority of cases it causes far greater psychological morbidity than physical symptoms. The most important part of medical management is to ensure the patient has access to accurate up to date information that can address their fears and provide them with tools to aid their understanding and to help them move on.
In this issue, Helpline nurse counsellor Claire Hurst QSM NZRN, addresses the question:
Herpes and pregnancy – what is the key information I should give to patients?
Getting a diagnosis of herpes can cause significant psychological morbidity, such as distress, worry and bewilderment.
Patients can feel too embarrassed and overwhelmed to ask questions of their medical practitioners. Commonly, people consult ‘Dr Google’ and read misleading and potentially detrimental information as the world wide web is full of misinformation, disinformation, and fraudulent herpes “cures”.
Please provide your patients with the www.herpes.org.nz link and/or the Helpline number: toll free from a land line 0508 11 12 13 or 09 433 6526 from a mobile.
Giving patients accurate up to date information at the time of diagnosis is as important as any medical management that is provided.
Women in particular worry about herpes and pregnancy and reassurance is very helpful.
Key information to provide patients regarding:
A diagnosis of genital herpes:
- Genital herpes does not affect fertility in women or men.
- Women can have normal pregnancies and vaginal deliveries.
- It is very rare to pass herpes onto babies.
- A woman with a history of genital herpes confers immunity to the baby because of maternal antibodies passing to the baby through the placenta.
- The greatest risk to the baby is when genital herpes (HSV 1 or HSV 2) is acquired for the first time in the last 3 months of pregnancy.
Prevention of herpes in pregnancy:
- All patients/couples who present should be asked about a history of oral or genital herpes and counselled accordingly about how to avoid transmission in the last 3 months of pregnancy.
- Most people are unaware that a primary episode of genital HSV 1, transmitted through oral to genital sex, can cause equally serious neonatal herpes as HSV 2, if acquired in the last trimester.
- Men who have a history of oral cold sores should be advised to avoid giving oral sex in the last trimester if their partner’s herpes antibody status is unknown.
- In the case of a discordant couple, where the male has genital or oral herpes, an antibody blood test for the partner may be helpful in determining the risk for the female. If no antibodies are present, then more caution is needed to avoid potential transmission.
For further information, refer to the NZHF website.
Aotearoa NZ STI Guidelines for Primary Care
The New Zealand Sexual Health Society (NZSHS), in collaboration with ASHM (Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine), has produced the Aotearoa New Zealand STI Guidelines for use in primary care settings. These were revised in 2021 and are now available at http://sti.guidelines.org.nz.
Note: These guidelines replace the STIEF and NZSHS Sexually Transmitted Infections Summary of Guidelines and feature new guidelines for ‘Populations and Situations’ and additional infections including:
- Bacterial Vaginosis
- Ectoparasites
- Hepatitis A, B & C
- HIV
- Mycoplasma genitalium
Conversations with young people about sex
STIEF board member, Dr Cathy Stephenson, recently presented ‘Conversations with young patients about sex’ in a Goodfellow podcast. Topics covered include:
- What do young people think about sex?
- How safe are our young people?
- Improving access for minority populations
- Free access to clinics
- Condom use
- Uptake of Gardasil vaccination
- Sexuality and gender identity
- Conversational tips and tricks
STI media mentions
'You may have chlamydia' email from University of Otago an unwelcome but welcome surprise
Sinead Gill
Stuff.co.nz Feb 10 2022
The first few weeks at university can be a petri dish for colds and flus, but catching a sexually transmitted infection can also be on the cards for unprepared students.
Much like Covid-19, contact tracing STIs was just as important as testing to stop the spread, though there was little formal funding for it, a sexual health expert said.
Luckily for students at the University of Otago, the university offered an anonymous messaging service to avoid the embarrassment or discomfort an STI-positive student may feel contacting sexual partners.
Who doesn't have it? International HPV Awareness Day
STIEF
Scoop Mar 2 2022
The 4th of March marks International HPV Awareness Day. This year’s international campaign theme is #onelessworry. The Human Papillomavirus, known as HPV, is one of the world’s most widespread viral infections, usually resulting from direct skin-to-skin contact during intimate sexual contact with someone who has HPV. The virus can be transmitted by penetrative as well as non-penetrative sexual contact and is thought to be the most common sexually transmitted infection in the world. In the case of sexually active adults, 80% of us are affected by HPV at some point in our lives - so - who doesn’t have it?